Temporal Lobe Epilepsy
1. Introduction: Temporal lobe epilepsy is a common type of refractory epilepsy. The etiology can be hippocampal sclerosis, developmental tumors, cortical dysplasia, cavernous hemangioma, trauma, infection, and some genetic factors. Overall, temporal lobe seizures can be characterized by behavioral arrest and impaired awareness, during the seizure oral and/or manual automatisms can occur. Some may have changes in sensory, emotional, cognitive, or autonomic function before consciousness is impaired. The impairment of consciousness in temporal lobe epilepsy is usually slower in onset and progression than in frontal lobe epilepsy, and postictal confusion is more pronounced. Ictal speech, spitting, vomiting, drinking, urge to urinate and automatisms with preserved consciousness suggest seizure onset in the non-dominant temporal lobe, whereas postictal speech disturbance suggests a dominant temporal lobe seizure. Upper limb dystonia is a useful lateralizing feature, often suggesting that seizures are located in the contralateral hemisphere, whereas manual automatisms usually occur on the ipsilateral side. In infantile temporal lobe epilepsy, seizures may be characterized by only pallor, apnea, and behavioral arrest, or earlier and moremarked motor manifestations, including tonic seizures and epileptic spasms [14].
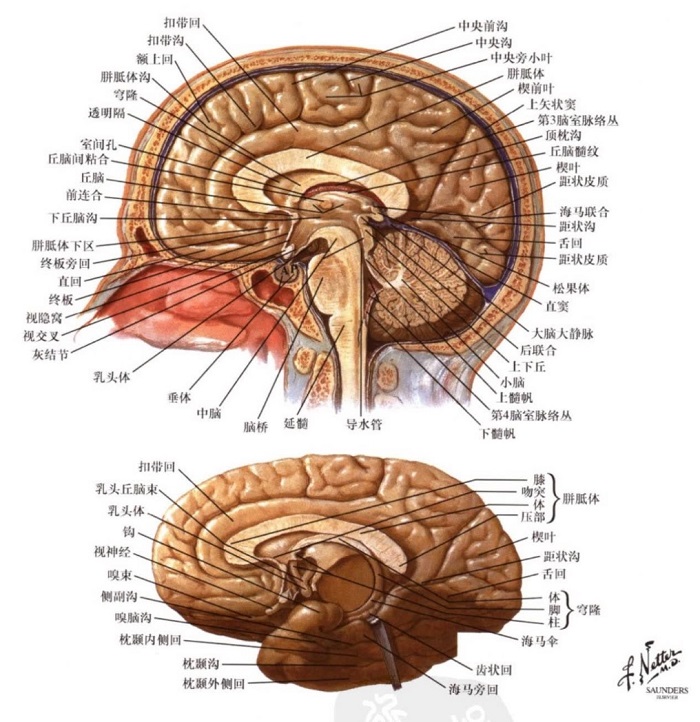
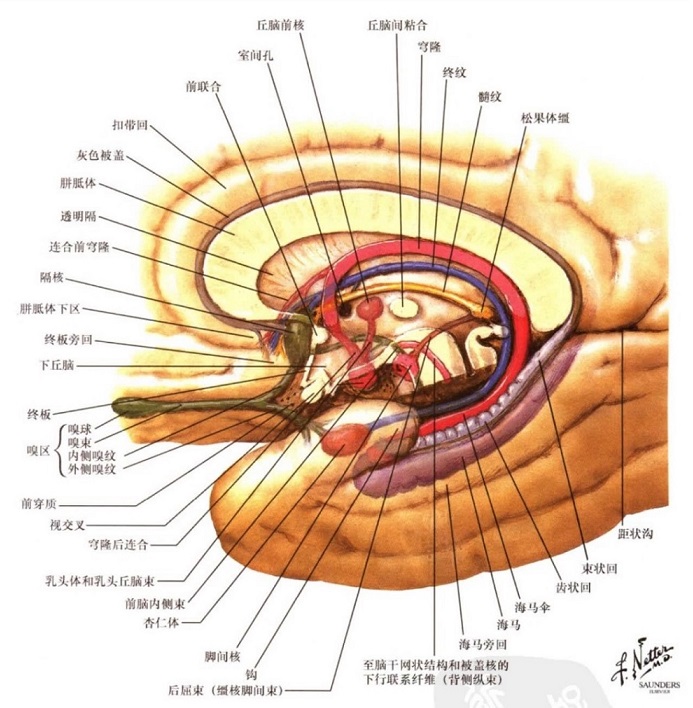
2. Temporal lobe anatomy [1-5]:
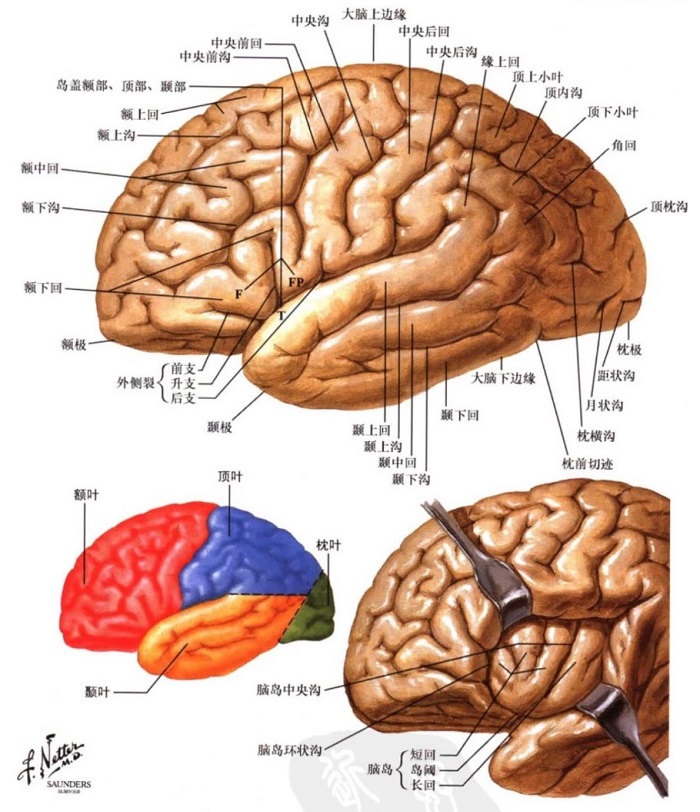
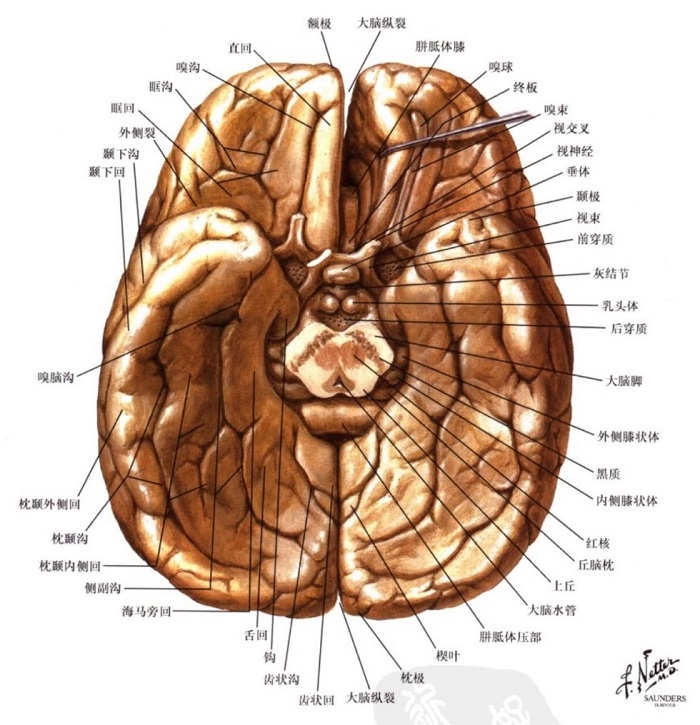
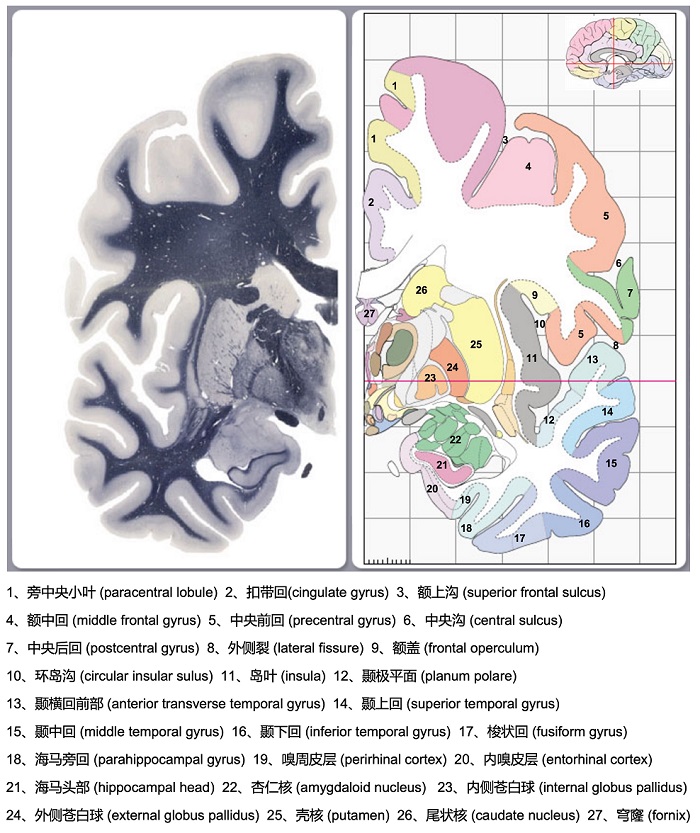
The temporal lobe is located below the sylvian fissure, and in front of the line connecting the upper edge of the parieto occipital sulcus and the anterior occipital notch. According to morphology, it can be divided into:
1. Dorsolateral: there are two sulcus parallel to the lateral fissure of the brain, namely superior temporal sulcus and middle temporal sulcus. The dorsolateral of the temporal lobe is divided into superior temporal gyrus, middle temporal gyrus and inferior temporal gyrus. Part of the superior temporal gyrus is covered into the lateral fissure, which is the transverse temporal gyrus.
2. Bottom and Medial: the bottom of the temporal lobe forms the anterior and middle part of the bottom of the brain. There are two sulcus from the outside to the inside, called occipito temporal sulcus and collateral sulcus. The lateral side of occipito temporal sulcus is the lateral occipitotemporal gyrus, which surrounds the lower edge of the hemisphere together with the inferior temporal gyrus. The medial occipitotemporal gyrus (also known as fusiform gyrus) is located on the inner side of the occipitotemporal sulcus. There are certain differences in the sources of different references here. In some references, the lateral occipitotemporal gyrus is equivalent to the fusiform gyrus. In other references, there is no statement of the lateral occipitotemporal gyrus and the medial occipitotemporal gyrus, it is considered that the fusiform gyrus is between the occipitotemporal sulcus and collateral sulcus. The medial side of the collateral sulcus (which can be connected to the flat and shallow rhina sulcus in the front of the temporal lobe) is the parahippocampal gyrus (also known as the hippocampal gyrus), the front end is curved, which is called the uncus, and its deep part has the amygdaloid body. The entorhinal cortex is also located in the anterior of the parahippocampal gyrus, and the medial side of the parahippocampal gyrus is the hippocampal sulcus, above the sulcus is a narrow strip of serrated cortex called dentate gyrus. From the inside, on the outside of the dentate gyrus, there is an arcuate uplift on the bottom wall of the lower corner of the lateral ventricle, which is called the hippocampus. The hippocampus and the dentate gyrus form the hippocampal formation.
3. The main functional areas of the temporal lobe [4, 6-7]:
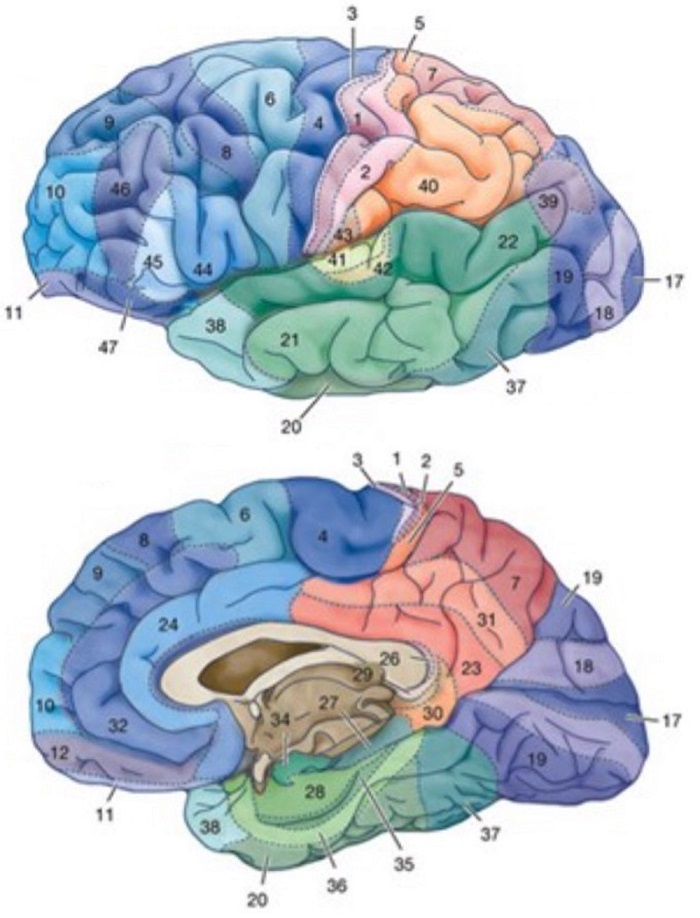
1. Sensory language area (Wernicke area, also known as auditory speech area): located in the posterior superior temporal gyrus of the dominant hemisphere (in Brodmann area 22), it can adjust own language and listen to and understand others' language. After the damage of this area, although the patient can hear others speak, he does not understand the meaning of the speech, and his own words are also incomprehensible. Therefore, he cannot correctly answer questions and speak normally, that is, sensory aphasia.
2. Auditory area: located in the middle of superior temporal gyrus and transverse temporal gyrus of bilateral hemispheres (mainly in Brodmann areas 41 and 42), it receives fibers from medial geniculate body, and each side receives impulses from both ears.
3. Olfactory area: located in and near the medial part of the parahippocampal gyrus (mainly in Brodmann area 34), receiving bilateral olfactory fibers.
4. Anterior temporal lobe: it is related to advanced neural activities such as memory, association and comparison.
5. Medial temporal lobe: related to memory, spirit, behavior and visceral function.
4、 Classification of temporal lobe epilepsy [8-10]:
According to the location of seizure onset, it can be divided into medial temporal lobe epilepsy (MTLE) and lateral temporal lobe epilepsy (LTLE, also known as neocortical temporal lobe epilepsy). Anatomically, the internal and external temporal lobes are divided mainly by the collateral sulcus, and the structures mainly contained in the medial temporal lobe include hippocampus, amygdala, parahippocampal gyrus and entorhinal cortex (located in the anterior segment of parahippocampal gyrus, which is listed separately because of its important function). The structures of lateral temporal lobe epilepsy mainly include superior temporal gyrus, middle temporal gyrus, inferior temporal gyrus and fusiform gyrus.
1. Medial temporal lobe epilepsy:
1)发作特点:常会有先兆,多数为上腹部先兆(如胃气上升感)、体验性先兆(如似曾相识感、陌生感、恐惧感等,有些会出现不愉快的嗅觉和味觉感受),有些随后会逐渐出现意识降低伴有口咽部自动症(包括咀嚼、吞咽、咂嘴等)或手部自动症(包括单手或双手的摸索、拍打、揉搓和抓握等),此外有些可出现自主神经功能障碍(出现心动过速、心动过缓、心律失常或出现呼吸暂停、呼吸过度等,有些可出现瞳孔散大,有时是不对称的,伴有对光反应消失、也可有瞳孔缩小,有些可出现流涎、脸红(但更常见的是脸色苍白)、尿失禁和竖毛等),有些可出现头眼向一侧偏斜(早期或偶发的头眼偏斜可能在致痫灶的同侧,后期的头偏斜常在病灶的对侧),以及出现对侧上肢的肌张力障碍。可持续数分钟,常有发作后意识混浊,之后意识逐渐恢复。一般很少继发全面-强直症挛发作。
2)脑电图表现:发作间期:可有前-中颞区及下颞区癫痫样放电,有些可向额区传导,部分可出现TIRDA。发作期:80%左右的患者在发作开始的30秒内可出现一侧性或局限于前下颞区的节律性5-9Hz的theta和alpha活动,节律性theta活动更常见于伴海马硬化颞叶内侧癫痫,有些内嗅皮层起源的也可以是低波幅快活的起始。约70%会出现发作后局部的慢波活动(如果存在约90%在发作起源的同侧),另外增加蝶骨电极以及10-20系统之外的下颞区电极(如T1/T2、F9/F10、T9/T10等)有助于发现间期和发作早起的放电。
2、外侧颞叶癫痫:
1)发作特点:可表现为听觉(如铃声、嗡嗡叫,碎裂声以及一些非特异性的噪音,如果只有一只耳朵听到,常表明癫痫发作起源于对侧半球)、视觉或前庭性先兆(同一患者可有多种先兆),涉及语言优势半球可出现言语障碍。由于颞叶外侧起源的发作可向内侧快速传导,有些随后可出现类似颞叶内侧型的自动症。此外由于外侧颞叶癫痫更容易向额叶皮质传导,运动症状如强直、阵挛(如面部肌肉的阵挛性动作)、偏转(可有整个身体旋转)以及继发全面-强直阵挛发作较内侧颞叶癫痫更常见。
2)脑电图表现:发作间期:可以是以中-后颞区放电为主。发作期:缺乏特异性,可表现为不规则delta活或低波幅快波活动,起始即可表现为双侧或一侧广泛性模式。
对于合并海马硬化的颞叶癫痫(temporal lobe epilepsy with hippocampal scerosis, TLE-HS),和海马有密切联系的其它边缘系统、旁边缘系统或新皮质结构也可能参与或独立成为颞叶癫痫的致痫灶,海马硬化可以因参与不同的颞叶癫痫网络而表现为不同的电-临床特征,可分为以下5个类型:
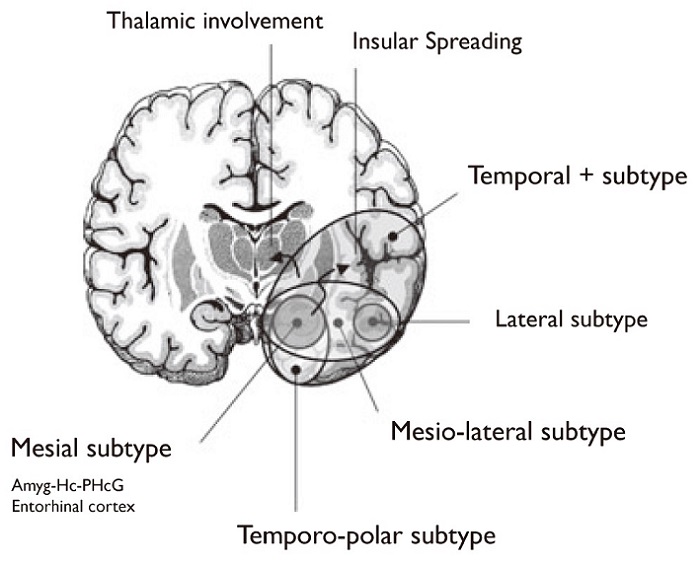
1、颞叶内侧型(mesial subtype):即伴海马硬化颞叶内侧癫痫,致痫灶位于颞叶内侧,除了硬化的海马外,杏仁核、海马旁回和内嗅区内嗅区也可各自独立或联合参与颞叶致痫区的形成,传导以颞叶新皮质、岛叶和眶额皮质等最为常见,患者常有典型的上腹部先兆或恐惧等体验性先兆,伴随口咽部自动症或手部自动症,其早期发作期脑电改变的范围较为局限,扩散到颞叶外区域相对较慢,癫痫发作时间较长。
2、颞极型(temporo-polar subtype):发作起源于颞极,或同时起源于颞极和海马,常优先传播至外侧裂周围皮质,患者意识损害较颞叶内侧型更早,早期发作期脑电改变也较为广泛。
3、颞叶内-外侧型(mesio-lateral subtype):患者的意识障碍和自动症迅速出现,发作更频繁,发作时间更长。
4、颞叶外侧型(Lateral subtype):单纯从颞叶外侧面起源(相对少见),患者易出现视听觉先兆、早期意识丧失癫痫发作时间短,容易继发全面强直-阵挛发作,也就上述外侧颞叶癫痫的表现。
5、颞叶癫痫附加症(temporal + subtype):其致痫网络同时包括颞叶及邻近结构如眶额皮质、岛叶、额叶岛盖部、顶叶岛盖部、颞顶枕交界处,这些患者中味幻觉、旋转性眩晕、竖毛、头眼向致痫灶对侧偏斜、同侧的强直发作、对侧肌张力障碍等症状出现的比例较其它类型高,发作后可有运动障碍。发作间期头皮脑电常出现双侧颞叶和颞叶外的癫痫样放电,发作期可出现颞叶外放电起始。
References
- 费尔腾. 奈特人体神经解剖彩色图谱. 北京 : 人民卫生出版社, 2006.
- Kucukyuruk, B., et al., Microsurgical anatomy of the temporal lobe and its implications on temporal lobe epilepsy surgery. Epilepsy Res Treat, 2012. 2012: p. 769825.
- 芮德源. 临床神经解剖学. 北京 : 人民卫生出版社, 2007.
- 柏树令. 系统解剖学. 第2版. 北京 : 人民卫生出版社, 2010.
- TheHumanBrain.info web (Accessed April 26, 2022).
- Dale Purves. Neuroscience fourth edition.Sinauer Associates Inc.,U.S., 2008.
- 贾建平. 神经病学. 北京 : 人民卫生出版社, 2019.
- Panayiotopoulos. 癫痫综合征及临床治疗. 北京 : 人民卫生出版社, 2012.
- 刘晓燕. 临床脑电图学. 第2版. 北京 : 人民卫生出版社, 2017.
- Maillard, L., et al., Semiologic and electrophysiologic correlations in temporal lobe seizure subtypes. Epilepsia, 2004. 45(12): p. 1590-9.
- Kahane, P. and F. Bartolomei, Temporal lobe epilepsy and hippocampal sclerosis: lessons from depth EEG recordings. Epilepsia, 2010. 51 Suppl 1: p. 59-62.
- 周永吉,朱露佳,王爽. 颞叶癫痫伴随海马硬化的研究进展[J]. 中华神经科杂志,2016,49(3):255-257.
- 张凯. 加深对颞叶癫痫的认识[J]. 中华神经外科杂志,2020,36(7):649-652.
- International League Against Epilepsy. temporal lobe seizure (Accessed April 28, 2022).

 English
English  简体中文
简体中文 